Boise parents often ask us how the PHP to IOP transition actually works and what it means for school, family time, and recovery. This guide explains the step-down process for teens in addiction treatment, answers common questions, and shows how you can support your child with confidence. Zelus Recovery serves families as a long-term partner across levels of care, from detox and partial hospitalization through outpatient aftercare, for both teens and adults in Boise.
What is partial hospitalization vs. intensive outpatient?
A partial hospitalization program (PHP) involves a structured treatment day with intensive care for teens who need more support than weekly therapy, yet do not require 24/7 inpatient care. Teens attend treatment for several hours on most weekdays, then return home in the evening. Programs include group therapy, individual therapy, family therapy, and medication management when appropriate.
Intensive outpatient programs (IOPs) are the next step down from PHPs. An intensive outpatient program offers multiple therapy sessions on select weekdays, often in the late afternoon or evening, so teens can manage daily responsibilities like school. IOP still includes individual therapy, group sessions, and skills practice, but with a lighter time commitment than PHP.
Intensive outpatient and partial hospitalization are both forms of outpatient care, designed to allow teens to receive treatment while still living at home.
At our partial hospitalization program, you can expect a safe and supportive environment, a focus on stabilization, and a plan that builds toward long-term recovery.
Key differences: PHP vs. IOP
- Time commitment: A partial hospitalization program runs for several hours most days, while intensive outpatient programs meet fewer days per week and for shorter blocks.
- Intensity: PHP provides more intensive treatment and more structured support, while IOP helps teens transition to practicing coping strategies in real life situations at home and at school.
- Medical oversight: PHP typically includes intensive psychiatric care and medication management check-ins, while IOP offers ongoing support with less frequent medical visits.
- School balance: PHP often begins with limited schoolwork, then IOP increases time for returning to class and extracurriculars as your teen stabilizes.
Learn more about our mental health and addiction treatment options for teens near Boise, ID.
Why the PHP to IOP step-down matters
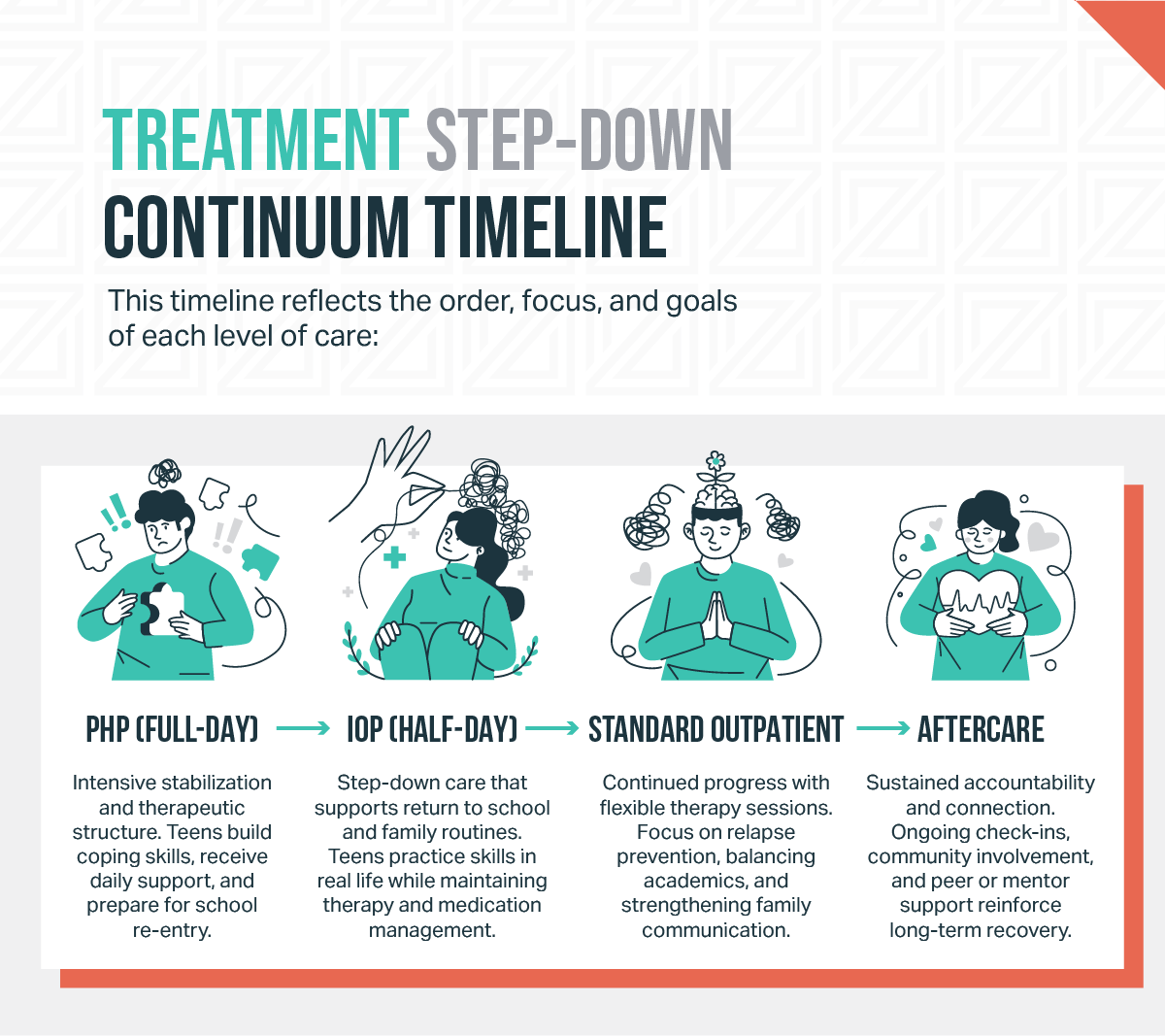
The step-down from a partial hospitalization program PHP to an intensive outpatient program is designed to match care with your teen’s progress. This transition reduces intensity in a planned way, which helps teens begin to apply new skills in their daily lives, build a strong support network, and continue mental health treatment without losing momentum.
Research on adolescent care emphasizes that behavioral therapies and family engagement are core to effective treatment. During the transition, teens continue evidence-based therapies, which can include cognitive behavioral approaches, dialectical behavior therapy, and family therapy components. Parents take an active role in coaching coping skills at home and shaping healthy routines that promote personal growth and a healthier future. These principles align with national guidance that highlights behavioral therapies, family involvement, and matching the level of care to the teen’s needs.
The goal of step-down care is not to “do less;” it is to right-size intensive support so teens can function independently with the right treatment at the right time. Carefully calibrated care transitions support long-term recovery, reduce relapse risk, and improve overall quality of life.
What parents can expect during the transition
Every teen’s treatment process is individualized. Length in a partial hospitalization program before moving to intensive outpatient depends on several factors, including safety, symptom stability, school readiness, and progress with therapeutic interventions. Teens move from PHP to IOP after a period of steady gains, when they can manage daily responsibilities with structured support.
Here is what the shift commonly includes:
- Comprehensive treatment plan review: The care team reviews goals, safety plans, school needs, and co-occurring disorders. Case management confirms community supports and coordinates with school counselors if needed.
- Schedule changes: PHP days gradually shorten, then IOP begins with treatment sessions clustered on fewer days. Families often notice that afternoons or evenings open up for school, activities, and family time.
- Therapy focus: Teens continue group therapy, individual therapy sessions, and family therapy at a frequency that fits IOP. Skills practice focuses on relapse prevention skills, distress tolerance, and emotion regulation.
- Medication management: Psychiatric care continues as needed. The team assesses response, side effects, and adherence, and makes adjustments carefully.
- Safety and supports: The team refreshes safety plans, confirms crisis contacts, and encourages a strong support network through mentors and community activities.
Overview:
- PHP: Attend treatment for several hours on most weekdays, with group therapy, individual counseling, family sessions, and supervised skills practice.
- IOP: Attend treatment on select weekdays, often later in the day, which allows your teen to attend school, complete assignments, and participate in extracurriculars.
If you have questions about how a schedule might look for your teen, talk with your care team about school start times, transportation, and extracurriculars. Your team will help tailor a plan that supports recovery and academics.
From Our Clients:
“Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat.”
-Name, City
Supporting your teen at home during step-down care
Parents are essential partners in step-down care. These practical steps help teens receive treatment while building independence:
- Set predictable routines: Keep consistent wake times, meal times, medication management, and electronics limits. Stability reduces stress and supports mental health.
- Use shared language: Ask your teen which coping strategies work best; for example, paced breathing, grounding, or a skills checklist from therapy sessions.
- Plan for triggers: Identify high-risk times, like late-night scrolling or certain social settings, and create alternatives such as exercise, art, or a check-in call with a trusted adult.
- Coordinate care: Track appointments, medication refills, and school deadlines. Case management can help organize support services and school notes.
- Encourage peer support: Safe friends and supervised activities help teens practice social skills and build confidence.
- Model calm problem solving: Teens learn from what we do. Use brief, clear steps: for example, name the problem, pick one next step, and check back in 15 minutes.
If substance use is part of your teen’s history, lock up medications and alcohol at home. Continue to use your family plan for monitoring, transportation, and rewards for healthy choices. When in doubt, ask the care team for more support.
School and social adjustments after PHP
Returning to school after partial hospitalization can feel like a big leap. However, many supports exist to ease the process, and thoughtful planning makes a real difference.
- Start with a school meeting: Include your teen, a counselor, and teachers. Share the plan for intensive outpatient, expected time away for treatment sessions, and any temporary academic adjustments.
- Consider accommodations: Some teens benefit from a lighter course load, extended time on tests, or a quiet testing space.
- Build connection: Feeling cared for at school protects mental health and reduces risky behaviors. School connectedness is linked to better mental health and fewer substance use risks.
- Rehearse social steps: Role-play how to answer questions from peers, how to leave an unsafe situation, and how to reach out to a school counselor.
- Keep activities on the calendar: Routines like sports, art, volunteering, or clubs support personal growth and structure.
Boise families can work with school counselors to align treatment schedules with classes and activities. Ask about quiet spaces for breaks, a point person for check-ins, and how to handle missed work during intensive outpatient treatment.
Talk to our team about your teen’s step-down plan
How Zelus Recovery supports teens through every level of care
Zelus Recovery partners with families through step-up and step-down care, focusing on continuity and clear communication. If your teen is stabilizing in a partial hospitalization program, our team helps you plan the step-down to intensive outpatient with attention to school re-entry, medication management, and family therapy involvement. We coordinate case management, confirm community referrals, and provide structured support that meets your teen’s changing needs.
Zelus Recovery stays with you as your teen transitions to outpatient care and aftercare. Our compassionate team collaborates with medical professionals, coordinates support services, and helps families maintain momentum toward a healthier future.






